Themen dieses Blogartikels:
Knowledge for your ears!
No time to read? Here you can listen to Claire's article.
What is Interval Hypoxia Hyperoxia Therapy (IHHT)?
Origins of IHHT: IHT and altitude training
Interval Hypoxia Hyperoxia Therapy is also known as Intermittent Hypoxia Hyperoxia Therapy or training. It starts in the area of energy metabolism and is therefore a kind of cell training or oxygen therapy. Central to IHHT are the different oxygen concentrations that are inhaled during the procedure.
In principle, IHT simulates altitude training at an altitude of about 2,000 meters. There, the air is, as they say, "thinner." This ultimately means that although the air at these altitudes has the same oxygen content as at sea level (20.95%), the air pressure up there is lower. So the higher you go up the mountain, the lower the air pressure and the less oxygen you take in through breathing (lower oxygen partial pressure).
This is noticeable! At airy heights, we find it harder to breathe and move. The resulting lack of oxygen is called hypoxia.

What are hypoxia and hyperoxia?
Hypoxia is by definition a lack of oxygen in the body and tissues, which leads to various adaptation mechanisms that can have a positive effect on energy supply. However, to induce hypoxia, one does not necessarily have to go to the mountains. One can also simulate it by breathing in a low level of oxygen through a mask. In addition to the phases with moderate hypoxia, in which little oxygen is inhaled, there are also phases in IHT in which oxygen is inhaled in the usual concentration (normoxic phases). Thus, there is alternation between the two phases. Hence the name interval hypoxia training.
IHHT can be seen as a further development of IHT and should lead to a faster recovery after hypoxia1,2. IHHT involves replacing periods of normal oxygenation with periods of high oxygenation. As a result, the patient breathes in more oxygen than usual and the body is supplied with more oxygen than usual. Consequently, exactly the opposite of hypoxia takes place here, namely hyperoxia. As with IHT, IHHT also alternates between the two phases.
IHHT procedure, duration and costs
Procedure
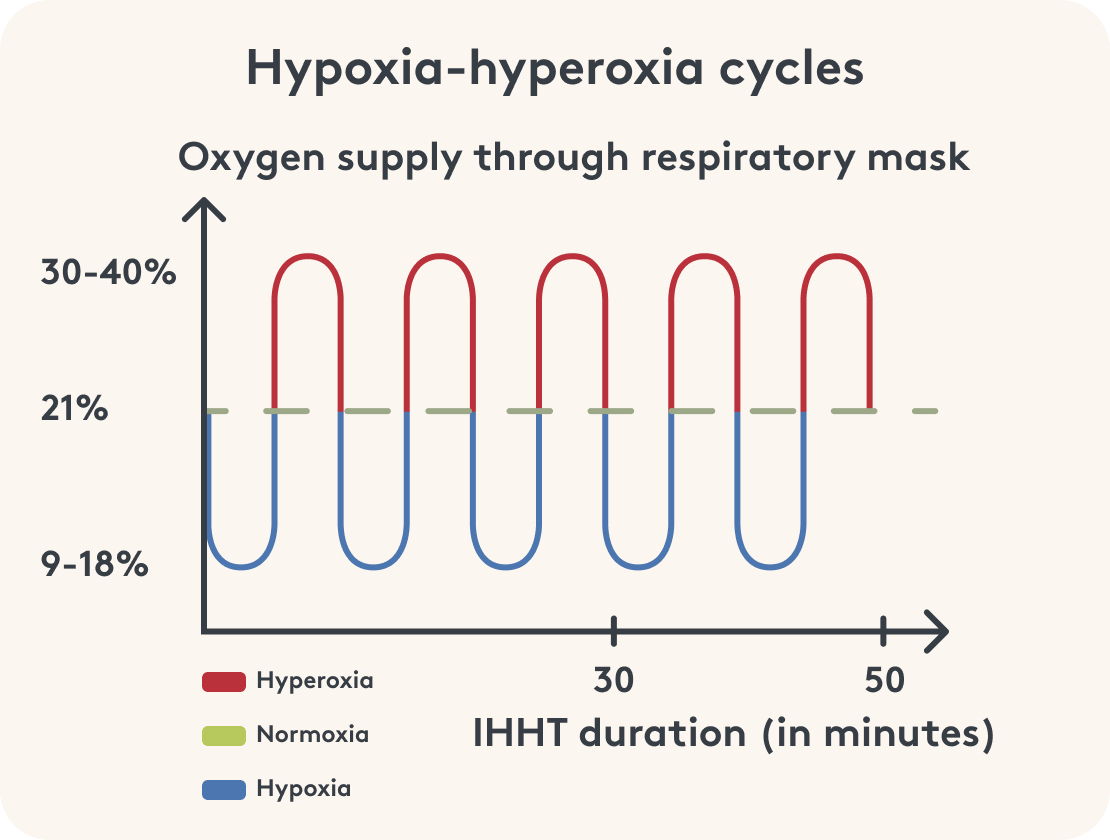
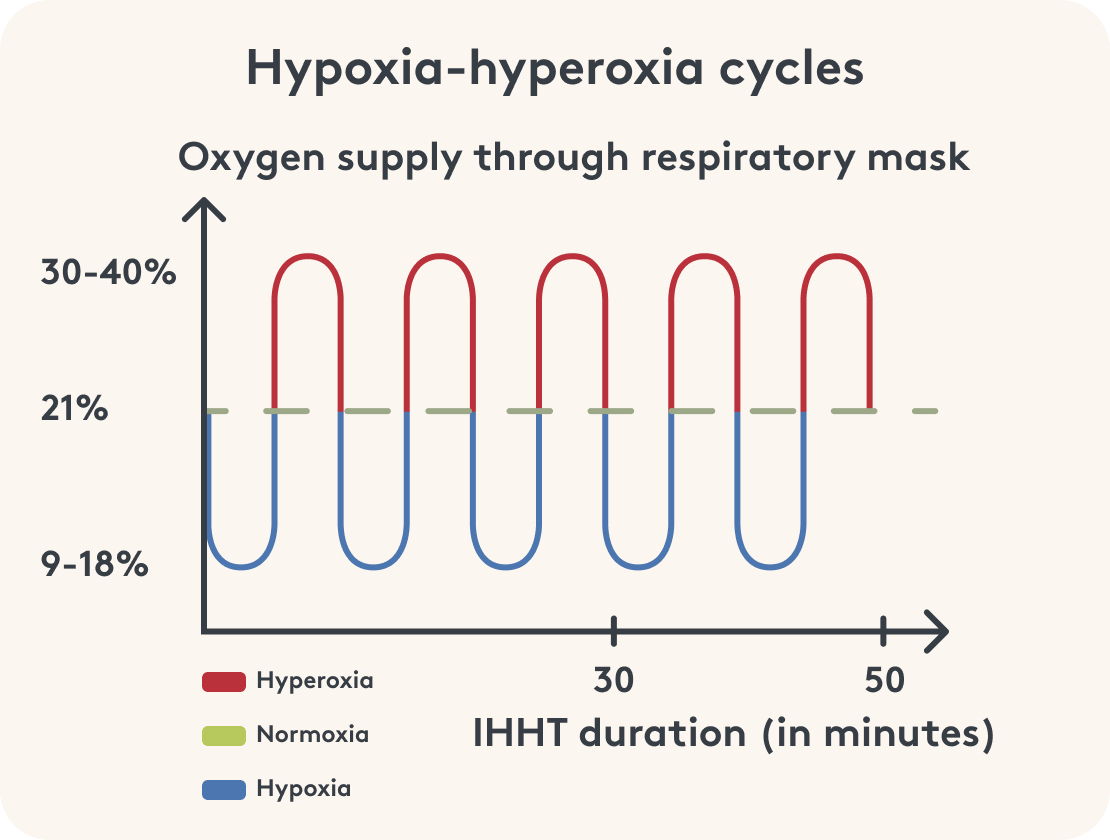
During an IHHT session, you will wear a breathing mask through which the appropriate amount of oxygen (O2) will be inhaled. Since IHHT is about hypoxia and hyperoxia, you will not breathe in air with the usual oxygen percentage of 20.95% through the breathing mask, but alternately low oxygen air (hypoxia: 9–18% O2) and high oxygen air (hyperoxia: 30–40% O2).
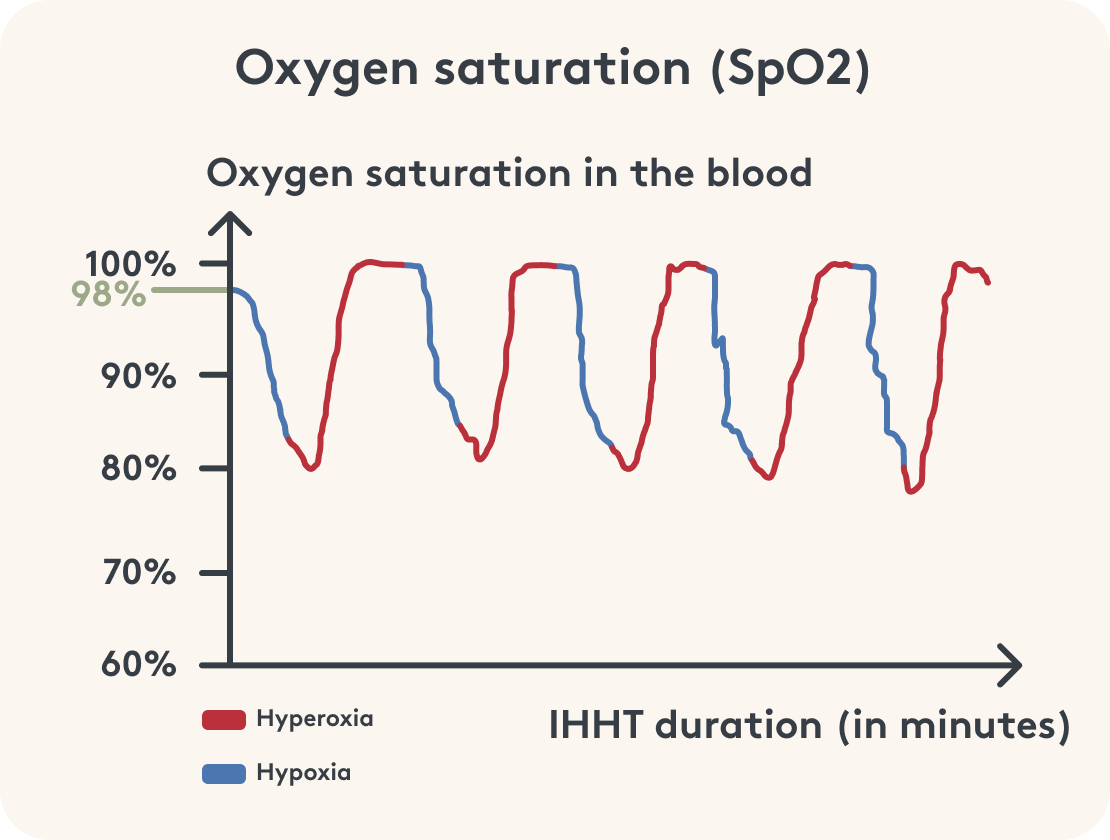
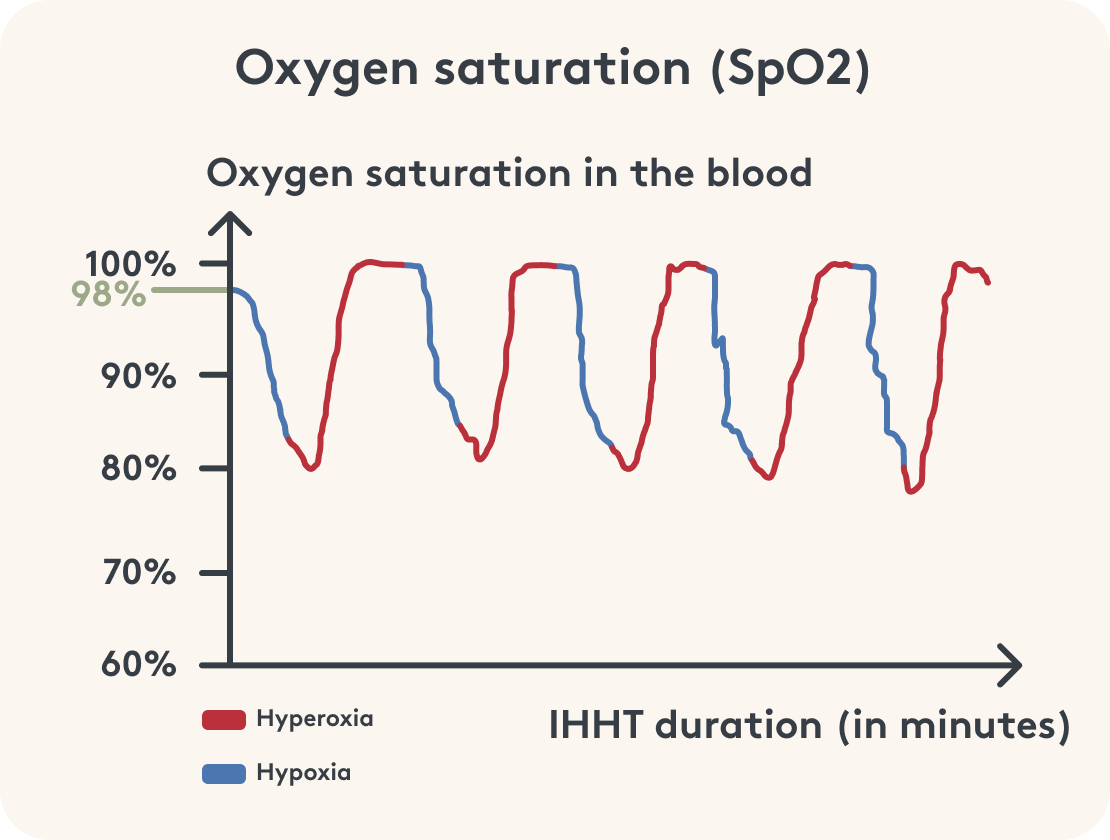
In addition to heart rate, or pulse, it also measures oxygen saturation (SpO2) in the arterial blood. It indicates how much oxygen is bound to the red blood pigment hemoglobin.
Under normal conditions in everyday life, your SpO2 is about 98%. During hypoxia, when little oxygen is inhaled, IHHT generally aims for an SpO2 of less than 90%. Depending on your health condition, your physical capacity and the available equipment, a range of 80-75% can also be achieved. During the following hypoxia, the phase with a lot of oxygen, values above the usual 98 % are aimed for. Accordingly 98-100 %.
Length of time
A hypoxia phase of 5 to 7 minutes is always followed by a hyperoxia phase. It is somewhat shorter at 2 to 4 minutes. The cycle of hypoxia-hyperoxia is repeated 3 to 5 times in total.
The duration of a single IHHT session depends on the length of the individual phases and the number of cycles. It is always possible to adjust it to your individual condition. The total length per session therefore varies between 30 and 50 minutes. A total of at least 10 sessions is recommended, although it has proven to be best to have 2 sessions per week.
Costs
The cost of IHHT therapy varies significantly. The price depends on the place where the therapy is carried out, on your initial condition, on the goal and therefore also on the total therapy duration. For about 60 € you can already get a trial session in some practices. Further sessions can often be booked as a package of 5 or 10. Here the IHHT costs per session are about 70-100 €.
Cost
The costs for IHHT therapy vary considerably. The price depends on the location, your initial condition, your goals, and therefore also on the overall duration of therapy.
In some practices, you can get a trial session for around €60. Additional sessions can often be booked as packages of 5 or 10. The IHHT costs per session range from approximately €70–100.
How does IHHT work?
IHHT can lead to various physical adaptation mechanisms over the long term. Depending on the mechanism, this can last several hours, days, or even weeks3.
Regeneration of mitochondria
The focus of IHHT is definitely on the mitochondria. What exactly are mitochondria? Simply explained, mitochondria are the powerhouses of your cells and are crucial for your energy metabolism. Without them, the provision of energy in the form of adenosine triphosphate (ATP) would be very limited. Some cells with very high energy requirements even contain up to 100,000 mitochondria. You can imagine that if the function of these small cell organelles is impaired and they work dysfunctionally, this can lead to enormous impairments in everyday life.
Mitochondria can reproduce themselves through direct division4. If the mitochondrial DNA (mtDNA) is damaged, the mitochondria become dysfunctional. This means they no longer function properly. When dysfunctional mitochondria divide, more dysfunctional mitochondria are created. This leads to further limitations in your energy supply5.


Regeneration of mitochondria
The focus of IHHT is definitely the mitochondria. What are mitochondria again exactly? Simply explained, mitochondria are the powerhouses of your cells and critical to your energy metabolism. Without them, the supply of energy in the form of adenosine triphosphate (ATP) would be very limited. In some cells with very high energy demands, there are even up to 100,000 mitochondria. You can imagine that if the function of these small cell organelles is limited and they work dysfunctionally, this can lead to enormous impairments in everyday life.
Mitochondria can self-replicate by direct division [4]. Should damage to mitochondrial DNA (mtDNA) occur, mitochondria become dysfunctional. That is, they no longer function properly. When the dysfunctional mitochondria divide, more dysfunctional mitochondria are then created. And that leads to further limitations in your energy supply5.
Damage to your mitochondria may be due to your lifestyle. For example, lack of sleep, poor diet, excess stress, or lack of exercise are all reasons for damaged mitochondria. On the other hand, aspects such as environmental toxins, viral infections, medications, and the normal aging process can also affect mitochondrial function4.
How do you notice that your mitochondria no longer perform what they once could, or actually could? It becomes clear especially with symptoms such as regular and persistent fatigue, low resilience, lack of energy and exhaustion.
But how can IHHT help in the area of mitochondria and energy supply?
IHHT can be seen as a way of mitochondrial therapy. Through the different administration of oxygen, sometimes a little, sometimes a lot, the mitochondria are exposed to stress. Not all mitochondria survive this, but only the well-functioning ones. The dysfunctional mitochondria die as a result. At the same time, this allows new young mitochondria to form1,6,7,8.
Advertisement
Over 40 micronutrients and plant substances
Wonderful all-rounder for your energy & performance
Numerous vitamins, amino acids, L-glutathione
More than 10 bioactive plant substances
Special blend for your fitness with coenzyme Q10
With biotin, thiamine, riboflavin, niacin, vitamin B12 & much more.
Developed with doctors & experts

But how can IHHT help in the area of mitochondria and energy production?
IHHT can be viewed as a potential form of mitochondrial therapy. Through varying amounts of oxygen, sometimes a little, sometimes a lot, the mitochondria are exposed to stress. Not all mitochondria survive this, but only the well-functioning ones. The dysfunctional mitochondria die as a result. At the same time, this allows new, young mitochondria to form1,6,7,8.
Further adaptation mechanisms
Due to the lack of oxygen, i.e., hypoxia, a number of other mechanisms in the body are triggered by the regulatory protein HIF (hypoxia-induced factor).3 These adaptations are primarily based on HIF responding to the low oxygen supply to maintain oxygen balance. Interval hypoxia-hyperoxia training (IHHT) achieves this by, on the one hand, making more oxygen available by producing more red blood cells that transport oxygen to the cells. On the other hand, new blood vessels are formed through which the oxygenated blood can flow.
On the other hand, HIF also reduces oxygen consumption by switching from oxidative metabolism (oxidative phosphorylation) to other energy production pathways that do not require oxygen.
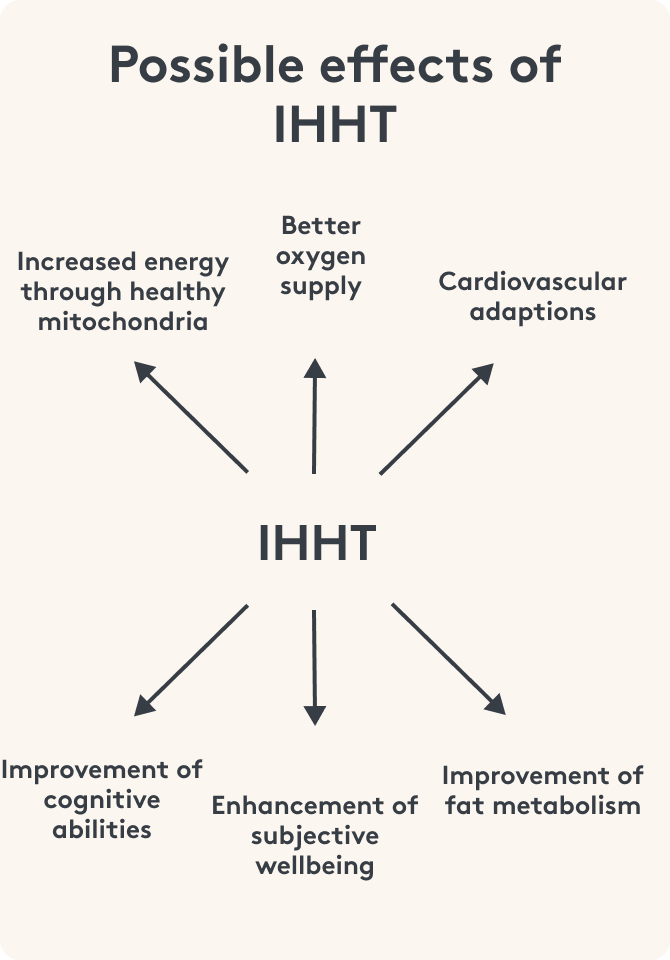
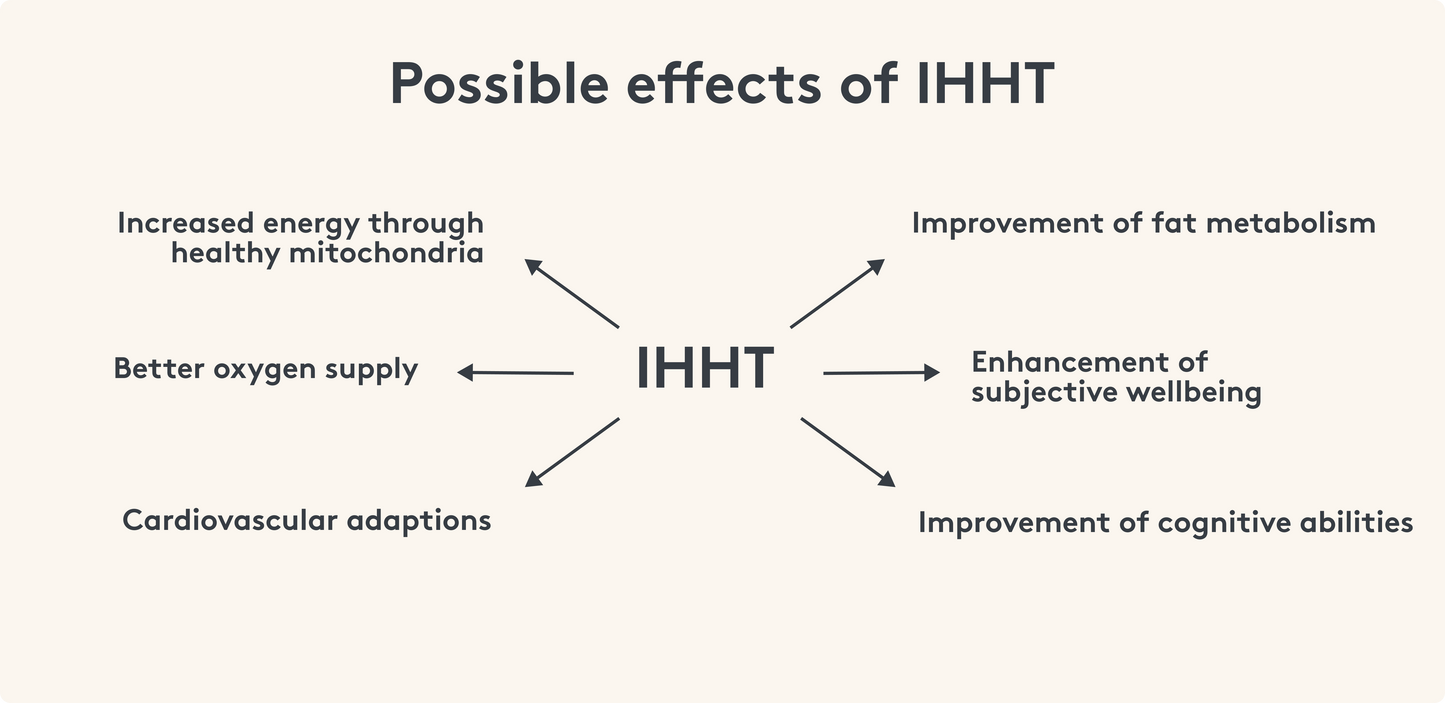
Other potential benefits of IHHT may include improvements in cardiovascular fitness, LDL cholesterol, body fat percentage, cognitive abilities, and subjective well-being.
Who can use IHHT?
Since IHHT is not a sport where you move and sweat, the training can also be a therapeutic approach for various diseases and indications. Examples are burn out, permanent fatigue and lack of energy, chronic diseases and lipometabolic disorders.
Of course, IHHT can also be used to enhance performance in sports10 or, in older age, to improve cognitive performance5,6.
How else can you strengthen your mitochondria?
Like all processes in our body, mitochondria require many building blocks in the form of nutrients to function properly. In addition to IHHT, an adequate supply of nutrients is also important. Because without building blocks, unfortunately, nothing can be built, including new energy. Therefore, special attention should be paid to the energy powerhouses of our cells.
This article is based on carefully researched sources:
Bibliography
2 Glazachev, O. S. (2013). Optimization of Clinical Application of Interval Hypoxic Training. Biomedical Engineering, 47(3), 134–137. https://doi.org/10.1007/s10527-013-9352-7
3 Prabhakar, N. R., & Semenza, G. L. (2015). Oxygen Sensing and Homeostasis. Physiology, 30(5), 340–348. https://doi.org/10.1152/physiol.00022.2015
4 Meyer, J. N., Leuthner, T. C., & Luz, A. L. (2017). Mitochondrial fusion, fission, and mitochondrial toxicity. Toxicology, 391, 42–53. https://doi.org/10.1016/j.tox.2017.07.019
5 Han, R., Liang, J., & Zhou, B. (2021). Glucose Metabolic Dysfunction in Neurodegenerative Diseases—New Mechanistic Insights and the Potential of Hypoxia as a Prospective Therapy Targeting Metabolic Reprogramming. International Journal of Molecular Sciences, 22(11), 5887. https://doi.org/10.3390/ijms22115887
6 Bayer, U., Likar, R., Pinter, G., Stettner, H., Demschar, S., Trummer, B., Neuwersch, S., Glazachev, O., & Burtscher, M. (2017). Intermittent hypoxic-hyperoxic training on cognitive performance in geriatric patients. Alzheimer’s & Dementia: Translational Research & Clinical Interventions, 3(1), 114–122. https://doi.org/10.1016/j.trci.2017.01.002
7 Serebrovska, T. V., Grib, O. N., Portnichenko, V. I., Serebrovska, Z. O., Egorov, E., & Shatylo, V. B. (2019). Intermittent Hypoxia/Hyperoxia Versus Intermittent Hypoxia/Normoxia: Comparative Study in Prediabetes. High Altitude Medicine & Biology, 20(4), 383–391. https://doi.org/10.1089/ham.2019.0053
8 Voronina, T., Grechko, N., Shikhlyarova, A., & Bobkova, N. (2017). Intermittent hypoxic training as an effective method of activation therapy. Cardiometry, 10, 93–99. https://doi.org/10.12710/cardiometry.2017.9399
9 Glazachev, O., Kopylov, P., Susta, D., Dudnik, E., & Zagaynaya, E. (2017). Adaptations following an intermittent hypoxia-hyperoxia training in coronary artery disease patients: A controlled study: Cardiopulmonary and metabolic adaptations after intermittent hypoxia-hyperoxia training. Clinical Cardiology, 40(6), 370–376. https://doi.org/10.1002/clc.22670
10 Susta, D., Dudnik, E., & Glazachev, O. S. (2017). A programme based on repeated hypoxia–hyperoxia exposure and light exercise enhances performance in athletes with overtraining syndrome: A pilot study. Clinical Physiology and Functional Imaging, 37(3), 276–281. https://doi.org/10.1111/cpf.12296











